Advances in technology and expanded payment have resulted in a dramatic increase in the adoption of diabetes devices such as continuous glucose monitors, blood glucose meters, and insulin pumps. These devices generate valuable patient data that can be used to elevate care.
At the same time, there are too many, disparate, diabetes device platforms which result in high cost for a health system to integrate into the EMR workflow. Device data acquisition, processing, interpreting, and documenting from all these device platforms create tremendous burden and workflow variability for clinicians and staff.

“My organization deals with many technology vendors. Care for patients with diabetes adds to this challenge due to all the disparate diabetes devices required for these patients. This new technology will not only improve clinical operations but reduce the need for multiple integrations and installations by the IT team.”
Lisa Stump
SVP, Chief Information and Digital Transformation Officer
Yale New Haven Health and Yale Medicine
To address this challenge, YNHHS deployed DreaMed’s endo.digital platform as an integrated part of the EMR workflow. The EMR integration included two components.
One, endo.digital was made accessible with one-click access directly from the patient record in the EMR. Providers did not need to sign in to a separate platform, and patient information was automatically pulled from the EMR. Two, data generated by the platform as part of the clinician workflow was automatically pushed back into discrete fields in the EMR visit record, into flowsheet and progress notes.

YNHHS partnered with DreaMed to devise a multi-phase deployment and measurement strategy and mobilize a cross-company / cross-functional project team to work elbow to elbow on the implementation as well as ongoing feedback, iterations, and enhancements.
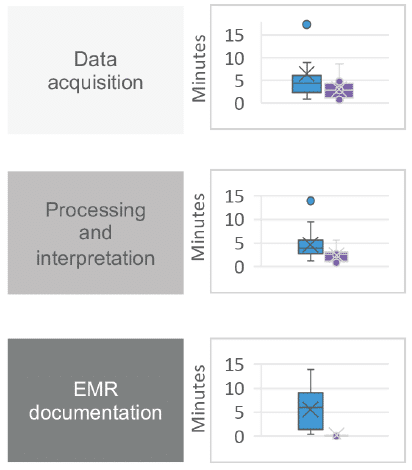
Success was measured in two phases. In the first phase, a time study was conducted on 3 clinicians at 3 different sites. Measurements included staff time invested and workflow process steps required for data acquisition, data interpretation, and post-visit documentation. In the second phase, the solution was deployed to all 15 staff members, at one clinic site, to measure clinician uptake. Measurements included the number of staff members using the platform, patient volume, and patient recommendations facilitated by the platform.
DreaMed’s
endo.digital platform
- Diabetes device data acquisition
- Diabetes data reports
- FDA cleared AI enhanced decision support
- Patient app and bolus calculator
- Automated payer billing documentation
8.9 minute reduction in time
required per patient visit
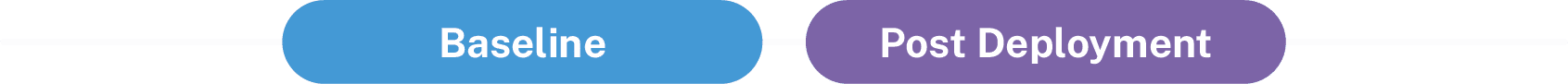
Printed pages per patient reduced to 0
Source: endo.digital time study at Northeast Medical Group Yale New Haven Health, Dec 2022 – Feb 2023, presented by Dr. Danielle Benaviv-Meskin at the ATTD in Berlin, February 2023
Yale New Haven Health
100% Clinician Uptake
- 7 out of 7 clinicians using the system weekly 5 months in a row
- 700+ patients onboarded
- 159 avg approved recommendations per month
Key Learnings
Collaborative spirit, transparency and having the right team in place are crucial. As an example, frequent and candid feedback directly from the users to the endo.digital team enabled rapid iterations and enhancements to the solution, both with technology features as well as service and support.
The degree of workflow variability and staff burden was even more pronounced than originally hypothesized. This was especially true of post-visit documentation. Diabetes devices generate a tremendous amount of data, that was creating not only a tremendous documentation burden but also dozens of printed pages per patient. This has a significant impact on the system's ability to bill and collect for the CGM review work being performed.
A whole team care approach is essential, where the technology and workflow is deployed to all staff and applicable patients. We learned that deployment to only select users and patients was not optimal, and in some instances created new barriers.